Breast Cancer
The Largest Breast Cancer Program in New Jersey
John Theurer Cancer Center is home to New Jersey’s largest breast cancer and breast imaging program, offering you a level of experience and expertise that’s unmatched across the state. We help you navigate your breast cancer diagnosis and treatment as a tight-knit team. As New Jersey's only nationally ranked cancer center by U.S. News & World Report 2025-2026, our globally recognized experts deliver the most effective and personalized breast cancer treatment options available.
Our breast health services include breast cancer diagnosis, treatment, support and survivorship navigators, as well as routine breast screenings and care for benign breast diseases. We also provide genetic counseling and testing and many other services for patients with high risk for breast cancer.
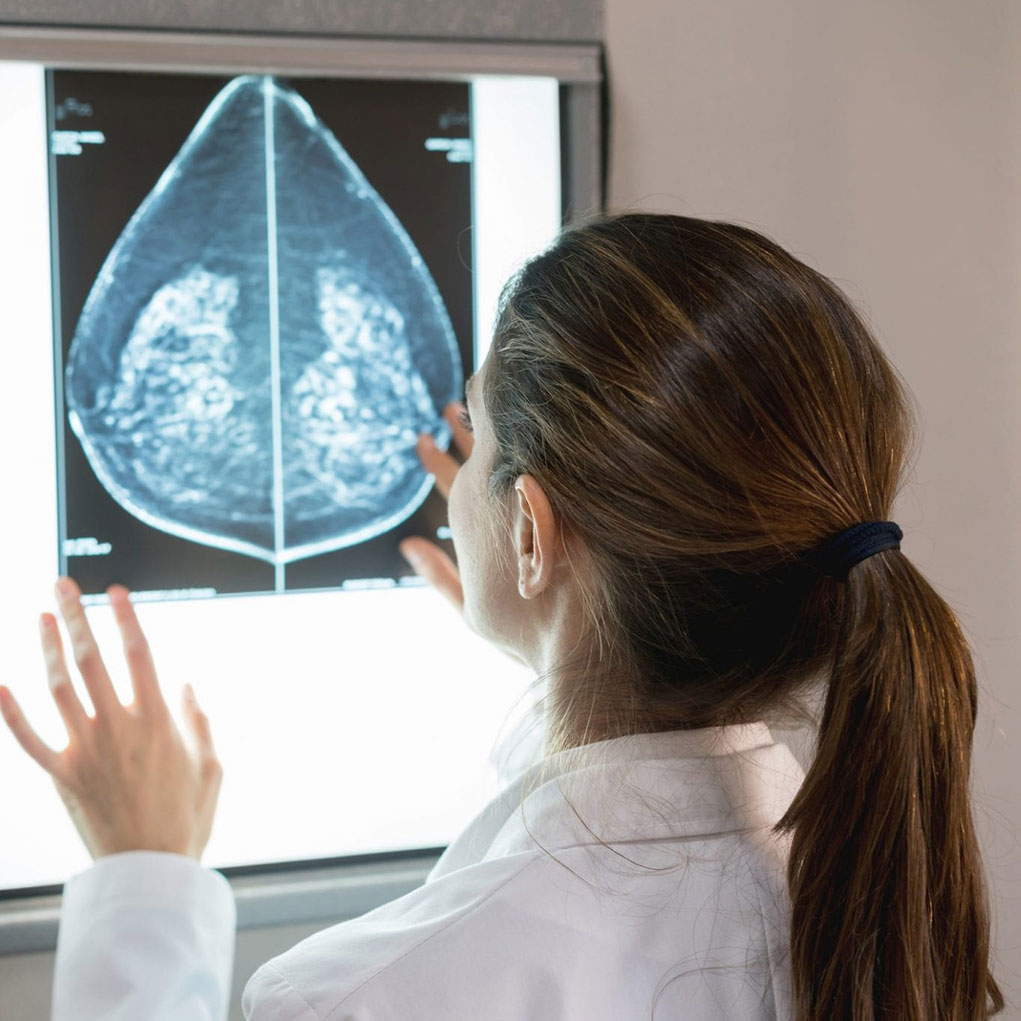
Screening and Diagnosis
Each of our imaging specialists have advanced training in breast imaging and only interpret breast images, providing them with laser-focused expertise. In addition to the services and resources below, view our Breast Health page for more information.
Find a Mammography Location Near You
Schedule a Mammogram Online
Also called digital breast tomosynthesis (DBT), this technology is more sensitive than conventional 2D mammography for detecting breast cancer, especially for women with dense breasts and even for women with fatty breasts.
This highly sensitive imaging is sometimes used in conjunction with mammography to screen women who have an elevated risk of breast cancer.
We use sound waves to image the breast and provide additional screening information.
If your breast imaging exams indicate that you need an ultrasound-guided biopsy, we can often provide a same-day biopsy.
If you had a screening or diagnostic mammogram at another facility, you can seek an additional assessment, biopsy, consultation or second opinion with our team of radiologists, surgeons and pathologists.
Our high-risk breast cancer program provides risk assessment and genetic testing for genes such as BRCA1 and BRCA2 so we can design follow-up and support care that is specific to your needs.
An advanced imaging technology that combines the benefits of high-resolution 3D mammography with functional imaging performed using a contrast agent. This form of mammography provides information about a tumor’s blood supply, which helps to improve breast cancer detection and imaging accuracy. This technology will allow women with dense breasts, personal or family history of breast cancer, genetic mutations, an abnormal mammogram result, concerning symptoms, or other conditions that increase breast cancer risk. The technology offers an advanced imaging alternative for women who cannot have breast MRI.
Treatment Options
Effective breast cancer treatment begins with a precise understanding of your specific tumor. Our approach to breast cancer care is centered on detailed tumor analysis, which allows us to identify the genetic and molecular characteristics of your cancer. This detailed profile guides your multidisciplinary team in developing a personalized treatment plan that may include targeted chemotherapy, hormonal therapy for ER+ or PR+ cancers, advanced radiation techniques, or a specific surgical approach.
Breast cancer treatments with Hackensack Meridian Health include:
- Chemotherapy
- Hormonal Therapy
- Radiation Therapy
- Breast Surgery
- Plastic Surgery
Screening FAQs
Treatment FAQs
- Chemotherapy and Personalized Treatment: We study your breast cancer tumor to identify genetic mutations and learn about the molecular signals involved in your breast cancer’s growth. We use the results to match you with breast cancer therapies that will best target the biology of your breast cancer.
- Hormonal Therapy: If lab tests determine that your breast cancer tumor is estrogen-positive (ER+) or progesterone-positive (PR+), this breast cancer treatment option can be used to block your body's natural hormones from reaching any remaining breast cancer cells.
- Accelerated (Hypofractionated) Radiation Therapy: Eligible patients can receive a higher dose of radiation delivered over a shorter overall treatment course, reducing the number of weeks you need to come in for treatment.
- Brachytherapy: This treatment involves temporary or permanent implantation of radioactive substances to kill breast cancer cells.
- Image-Guided Radiation Therapy (IGRT): We take images of your breast cancer tumor before each treatment so we can customize the radiation to the breast cancer tumor’s size and shape as it shrinks and changes position, giving you only the dose you need and reducing exposure to noncancerous tissues.
- Intensity-Modulated Radiation Therapy (IMRT): IMRT directs radiation of various intensities, shaped to the contours of a breast cancer tumor, from a variety of angles to destroy tumor tissue while sparing normal breast tissue as much as possible.
- Prone Radiation Therapy: This advanced breast cancer treatment allows us to direct radiation to the breast while sparing lung and heart tissue and reducing the risk of late-term side effects.
Our breast surgeons are nationally recognized experts with extensive experience in every type of breast cancer surgery.
- Lumpectomy: This breast-conserving surgery removes the portion of the breast that contains the cancer, and some surrounding normal tissue.
- Mastectomy: The entire breast is removed, including all of the breast tissue. If both breasts are removed, this is called a double mastectomy.
Post-Treatment FAQs
Our breast reconstruction surgeons are skilled in the latest plastic and reconstructive surgery techniques, including breast implants and flap reconstruction procedures—groundbreaking breast reconstructive surgeries that require surgical expertise.
Our Research and Clinical Trials
At Hackensack Meridian Health, you may have the opportunity to participate in a clinical trial of new and exciting approaches to stem cell transplant. Our research has a strong focus on reducing the complications of transplant and also lowering the risk of disease recurrence. We are the first in the world to combine checkpoint inhibitors (drugs that inhibit the proteins cancer cells use to evade detection by the immune system) after transplantation, at a time when the immune system has the best opportunity to eliminate any remaining cancer cells.